The Nobel Prize in Physiology or Medicine 2023
来源:The nobelprize官网 | 发布时间:2023-10-02
The Nobel Assembly at Karolinska Institutet has today decided to award the 2023 Nobel Prize in Physiology or Medicine jointly to Katalin Karikó and Drew Weissman.
for their discoveries concerning nucleoside base modifications that enabled the development of effective mRNA vaccines against COVID-19.
The discoveries by the two Nobel Laureates were critical for developing effective mRNA vaccines against COVID-19 during the pandemic that began in early 2020. Through their groundbreaking findings, which have fundamentally changed our understanding of how mRNA interacts with our immune system, the laureates contributed to the unprecedented rate of vaccine development during one of the greatest threats to human health in modern times.
Vaccines before the pandemic
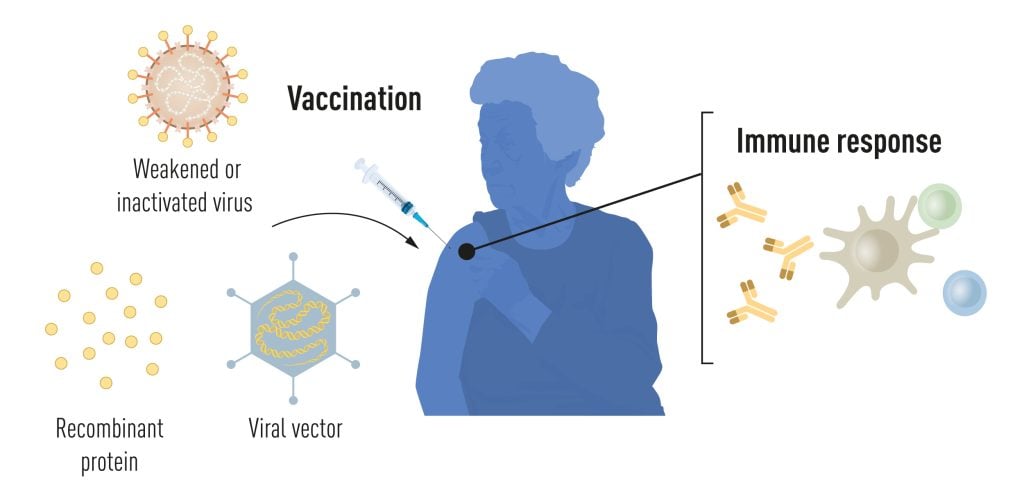
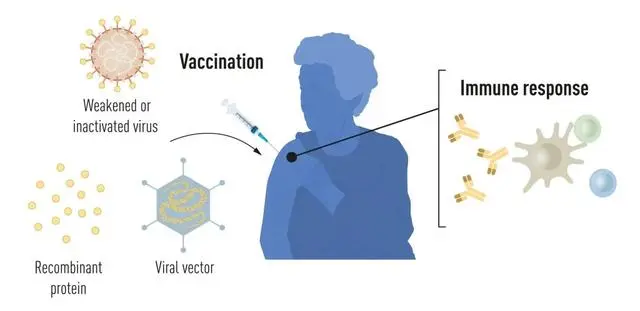
Vaccination stimulates the formation of an immune response to a particular pathogen. This gives the body a head start in the fight against disease in the event of a later exposure. Vaccines based on killed or weakened viruses have long been available, exemplified by the vaccines against polio, measles, and yellow fever. In 1951, Max Theiler was awarded the Nobel Prize in Physiology or Medicine for developing the yellow fever vaccine.
Thanks to the progress in molecular biology in recent decades, vaccines based on individual viral components, rather than whole viruses, have been developed. Parts of the viral genetic code, usually encoding proteins found on the virus surface, are used to make proteins that stimulate the formation of virus-blocking antibodies. Examples are the vaccines against the hepatitis B virus and human papillomavirus. Alternatively, parts of the viral genetic code can be moved to a harmless carrier virus, a “vector.” This method is used in vaccines against the Ebola virus. When vector vaccines are injected, the selected viral protein is produced in our cells, stimulating an immune response against the targeted virus.
Producing whole virus-, protein- and vector-based vaccines requires large-scale cell culture. This resource-intensive process limits the possibilities for rapid vaccine production in response to outbreaks and pandemics. Therefore, researchers have long attempted to develop vaccine technologies independent of cell culture, but this proved challenging.
mRNA vaccines: A promising idea
In our cells, genetic information encoded in DNA is transferred to messenger RNA (mRNA), which is used as a template for protein production. During the 1980s, efficient methods for producing mRNA without cell culture were introduced, called in vitro transcription. This decisive step accelerated the development of molecular biology applications in several fields. Ideas of using mRNA technologies for vaccine and therapeutic purposes also took off, but roadblocks lay ahead. In vitro transcribed mRNA was considered unstable and challenging to deliver, requiring the development of sophisticated carrier lipid systems to encapsulate the mRNA. Moreover, in vitro-produced mRNA gave rise to inflammatory reactions. Enthusiasm for developing the mRNA technology for clinical purposes was, therefore, initially limited.
These obstacles did not discourage the Hungarian biochemist Katalin Karikó, who was devoted to developing methods to use mRNA for therapy. During the early 1990s, when she was an assistant professor at the University of Pennsylvania, she remained true to her vision of realizing mRNA as a therapeutic despite encountering difficulties in convincing research funders of the significance of her project. A new colleague of Karikó at her university was the immunologist Drew Weissman. He was interested in dendritic cells, which have important functions in immune surveillance and the activation of vaccine-induced immune responses. Spurred by new ideas, a fruitful collaboration between the two soon began, focusing on how different RNA types interact with the immune system.
The breakthrough
Karikó and Weissman noticed that dendritic cells recognize in vitro transcribed mRNA as a foreign substance, which leads to their activation and the release of inflammatory signaling molecules. They wondered why the in vitro transcribed mRNA was recognized as foreign while mRNA from mammalian cells did not give rise to the same reaction. Karikó and Weissman realized that some critical properties must distinguish the different types of mRNA.
RNA contains four bases, abbreviated A, U, G, and C, corresponding to A, T, G, and C in DNA, the letters of the genetic code. Karikó and Weissman knew that bases in RNA from mammalian cells are frequently chemically modified, while in vitro transcribed mRNA is not. They wondered if the absence of altered bases in the in vitro transcribed RNA could explain the unwanted inflammatory reaction. To investigate this, they produced different variants of mRNA, each with unique chemical alterations in their bases, which they delivered to dendritic cells. The results were striking: The inflammatory response was almost abolished when base modifications were included in the mRNA. This was a paradigm change in our understanding of how cells recognize and respond to different forms of mRNA. Karikó and Weissman immediately understood that their discovery had profound significance for using mRNA as therapy. These seminal results were published in 2005, fifteen years before the COVID-19 pandemic.
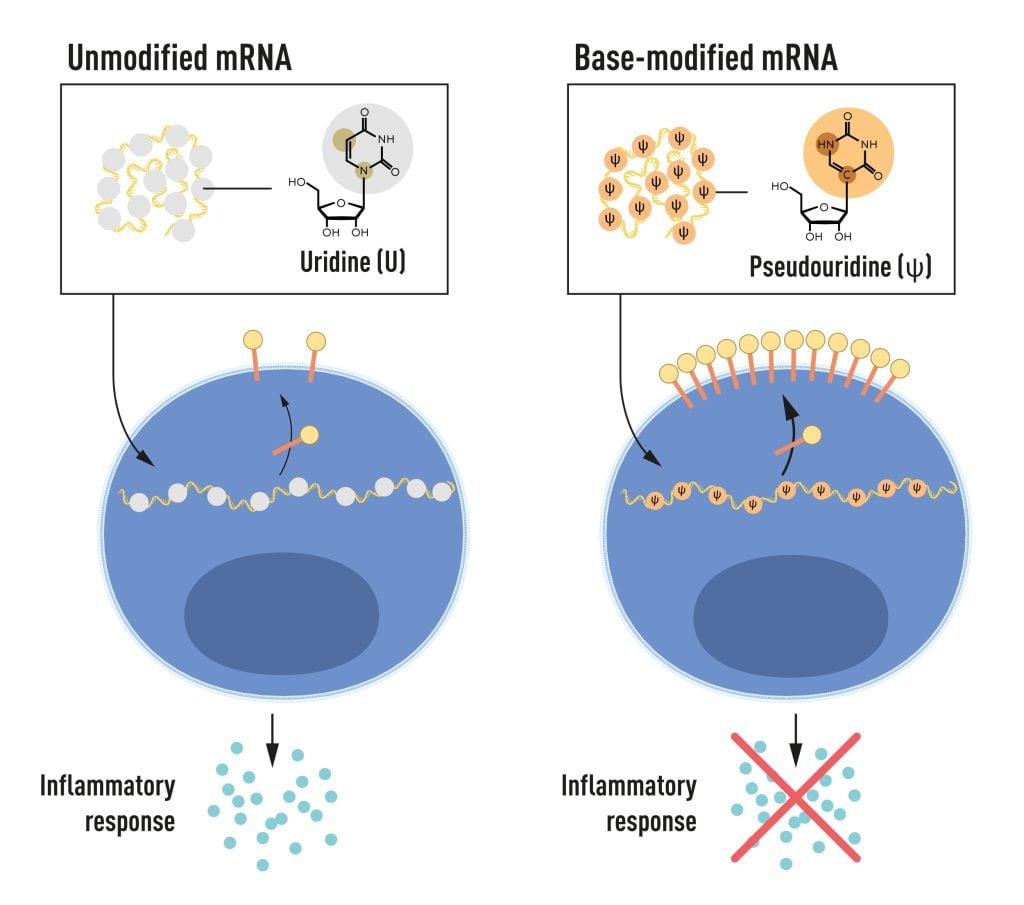
In further studies published in 2008 and 2010, Karikó and Weissman showed that the delivery of mRNA generated with base modifications markedly increased protein production compared to unmodified mRNA. The effect was due to the reduced activation of an enzyme that regulates protein production. Through their discoveries that base modifications both reduced inflammatory responses and increased protein production, Karikó and Weissman had eliminated critical obstacles on the way to clinical applications of mRNA.
mRNA vaccines realized their potential
Interest in mRNA technology began to pick up, and in 2010, several companies were working on developing the method. Vaccines against Zika virus and MERS-CoV were pursued; the latter is closely related to SARS-CoV-2. After the outbreak of the COVID-19 pandemic, two base-modified mRNA vaccines encoding the SARS-CoV-2 surface protein were developed at record speed. Protective effects of around 95% were reported, and both vaccines were approved as early as December 2020.
The impressive flexibility and speed with which mRNA vaccines can be developed pave the way for using the new platform also for vaccines against other infectious diseases. In the future, the technology may also be used to deliver therapeutic proteins and treat some cancer types.
Several other vaccines against SARS-CoV-2, based on different methodologies, were also rapidly introduced, and together, more than 13 billion COVID-19 vaccine doses have been given globally. The vaccines have saved millions of lives and prevented severe disease in many more, allowing societies to open and return to normal conditions. Through their fundamental discoveries of the importance of base modifications in mRNA, this year’s Nobel laureates critically contributed to this transformative development during one of the biggest health crises of our time.
Key publications
Karikó, K., Buckstein, M., Ni, H. and Weissman, D. Suppression of RNA Recognition by Toll-like Receptors: The impact of nucleoside modification and the evolutionary origin of RNA. Immunity 23, 165–175 (2005).
Karikó, K., Muramatsu, H., Welsh, F.A., Ludwig, J., Kato, H., Akira, S. and Weissman, D. Incorporation of pseudouridine into mRNA yields superior nonimmunogenic vector with increased translational capacity and biological stability. Mol Ther 16, 1833–1840 (2008).
Anderson, B.R., Muramatsu, H., Nallagatla, S.R., Bevilacqua, P.C., Sansing, L.H., Weissman, D. and Karikó, K. Incorporation of pseudouridine into mRNA enhances translation by diminishing PKR activation. Nucleic Acids Res. 38, 5884–5892 (2010).
Katalin Karikó was born in 1955 in Szolnok, Hungary. She received her PhD from Szeged’s University in 1982 and performed postdoctoral research at the Hungarian Academy of Sciences in Szeged until 1985. She then conducted postdoctoral research at Temple University, Philadelphia, and the University of Health Science, Bethesda. In 1989, she was appointed Assistant Professor at the University of Pennsylvania, where she remained until 2013. After that, she became vice president and later senior vice president at BioNTech RNA Pharmaceuticals. Since 2021, she has been a Professor at Szeged University and an Adjunct Professor at Perelman School of Medicine at the University of Pennsylvania.
Drew Weissman was born in 1959 in Lexington, Massachusetts, USA. He received his MD, PhD degrees from Boston University in 1987. He did his clinical training at Beth Israel Deaconess Medical Center at Harvard Medical School and postdoctoral research at the National Institutes of Health. In 1997, Weissman established his research group at the Perelman School of Medicine at the University of Pennsylvania. He is the Roberts Family Professor in Vaccine Research and Director of the Penn Institute for RNA Innovations.
2023年诺贝尔生理学或医学奖揭晓,mRNA疫苗技术斩获殊荣
近日,“2023年诺贝尔生理学或医学奖”获奖名单揭晓。瑞典斯德哥尔摩卡罗林斯卡学院(Karolinska Institute)的诺贝尔大会宣布,将该奖项授予美国科学家卡塔林·卡里科(Katalin Karikó)和德鲁·魏斯曼(Drew Weissman),因为他们发现了核苷酸基修饰,从而开发出有效的mRNA疫苗。他们将共享1100万瑞典克朗奖金(约合732万元人民币)。
诺贝尔奖委员会表示,今年的获奖者通过他们的突破性发现从根本上改变了我们对mRNA如何与免疫系统相互作用的理解。在现代人类健康面临的最大威胁之一期间,它们为疫苗前所未有的开发速度做出了贡献。
mRNA分子由四种核苷基组成,分别是adenine(A)、guanine(G)、cytosine(C)和uracil(U)。核苷基修饰就是在这四种核苷基上进行化学官能团的添加或去除,从而改变核苷基的化学性质。
诺贝尔奖新闻稿中写道:两位诺贝尔奖得主的发现,对于在2020年初开始的疫情期间开发出有效的新冠肺炎mRNA疫苗至关重要。通过他们开创性的发现,根本改变了我们对mRNA与免疫系统互动的理解,两位获奖者在现代对人类健康的最大威胁之一期间,对疫苗开发的空前速度做出了贡献。
凭借在新冠疫苗研发方面的贡献,两位科学家此前已获得了多项大奖,包括2022年美国科学突破奖(Breakthrough Prize)、2021年拉斯克基础医学研究奖(The Lasker Awards)、2023年盖尔德纳奖等。其中,拉斯克奖被视为诺贝尔生理学或医学奖的“风向标”。
另外,两位科学家将平均分享1100万瑞典克朗的奖金(约合715万元人民币)。相较于往年的1000万瑞典克朗,今年的诺贝尔奖奖金增加了100万瑞典克朗(约合65万元人民币)。
包括今年在内,共有225名科学家获得过诺贝尔生理学或医学奖,Katalin Kariko教授是第13位获得该奖的女性科学家。
消除mRNA关键障碍
资料显示,Katalin Kariko是塞格德大学教授和宾夕法尼亚大学佩雷尔曼医学院兼职教授,曾担任BioNTech RNA Pharmaceuticals副总裁和高级副总裁。
Kariko于1982年从匈牙利著名学府塞格德大学获得博士学位,1985年移居美国,专门从事研究RNA及其化学合成,即在体外合成mRNA,再将其引入细胞内,使其产生新的蛋白质。
Drew Weissman现任宾夕法尼亚州佩雷尔曼医学院罗伯茨家族疫苗研究教授。1997年,他在该大学开办了实验室主要研究开发HIV疫苗。与Kariko合作之后,他开始投入以mRNA作为疫苗的研究。
很久以来,mRNA技术应用的最大障碍是,体外转录的mRNA会被树突状细胞识别为外来物质,进一步引发免疫细胞的激活,以及炎症信号分子的释放。但体内的mRNA可以避免这种情况。
Kariko和Weissman发现,体内的mRNA结构上有一些化学修饰,能够使其避免免疫系统的攻击。
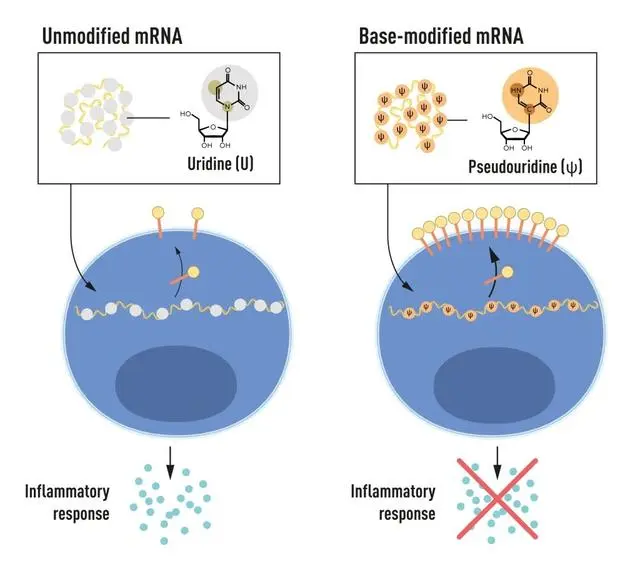
mRNA 包含四种不同碱基,缩写分别为 A、U、G、C。诺贝尔奖获得者发现了核苷碱基修饰后的 mRNA 可以用来阻断炎症反应的激活(信号分子的分泌),并增加 mRNA 传送至细胞时的蛋白质合成。随后,他们将化学修饰应用到mRNA上,结果出乎意料的好:当mRNA中包含碱基修饰时,能成功躲避免疫系统的攻击,非预期炎症反应也基本消失。
2005年,也就是新冠疫情爆发的十五年前,Kariko和Weissman发表了关于核苷基修饰的RNA是非免疫原性的论文,在业内引发了强烈反响。
在2008年和2010年发布的后续研究中,Kariko和Weissman还发现,相比未修饰的mRNA,碱基修饰后的mRNA可以显著增加蛋白合成。至此,mRNA技术临床应用中的两大关键障碍被消除。
mRNA不止被应用到新冠上
也就在2010年,多家公司开始致力于开发mRNA疫苗技术,研发针对寨卡病毒和中东呼吸综合征冠状病毒的疫苗,后者与SARS-CoV-2(新型冠状病毒)密切相关。
2020年疫情爆发后,开发人员以破纪录的速度开发出了两种编码SARS-CoV-2表面蛋白的碱基修饰mRNA疫苗,并在同年12月获得了批准。
报道显示,这两种疫苗的保护效果约为95%,全球抗疫战争迎来了崭新的局面。
不仅如此,mRNA疫苗开发的灵活性和速度,为将其他传染病的疫苗开发铺平了道路。未来,该技术还可用于递送治疗蛋白和治疗某些类型的癌症。